State officials expect virus to take greater toll on racial minorities

Go Deeper.
Create an account or log in to save stories.
Like this?
Thanks for liking this story! We have added it to a list of your favorite stories.
Minnesota has some of the worst health disparities in the nation, so state officials are not celebrating the state’s outbreak data which, so far, doesn’t reveal significant racial differences in hospitalizations or deaths.
African Americans, who make up about 7 percent of the state’s population, currently account for 3 percent of the state’s COVID-19 fatalities, according to the Minnesota Department of Health.
Earlier this month, state Health Commissioner Jan Malcolm said a significant portion of people who tested positive chose not to identify with any racial or ethnic category, so that can make it difficult to know if there are disparities. She said state officials are paying close attention to how the virus affects people of color.
“Because as is so true with just about every health issue we know, the burden of COVID-19 does not fall evenly or equitably in all communities,” she said.
Turn Up Your Support
MPR News helps you turn down the noise and build shared understanding. Turn up your support for this public resource and keep trusted journalism accessible to all.
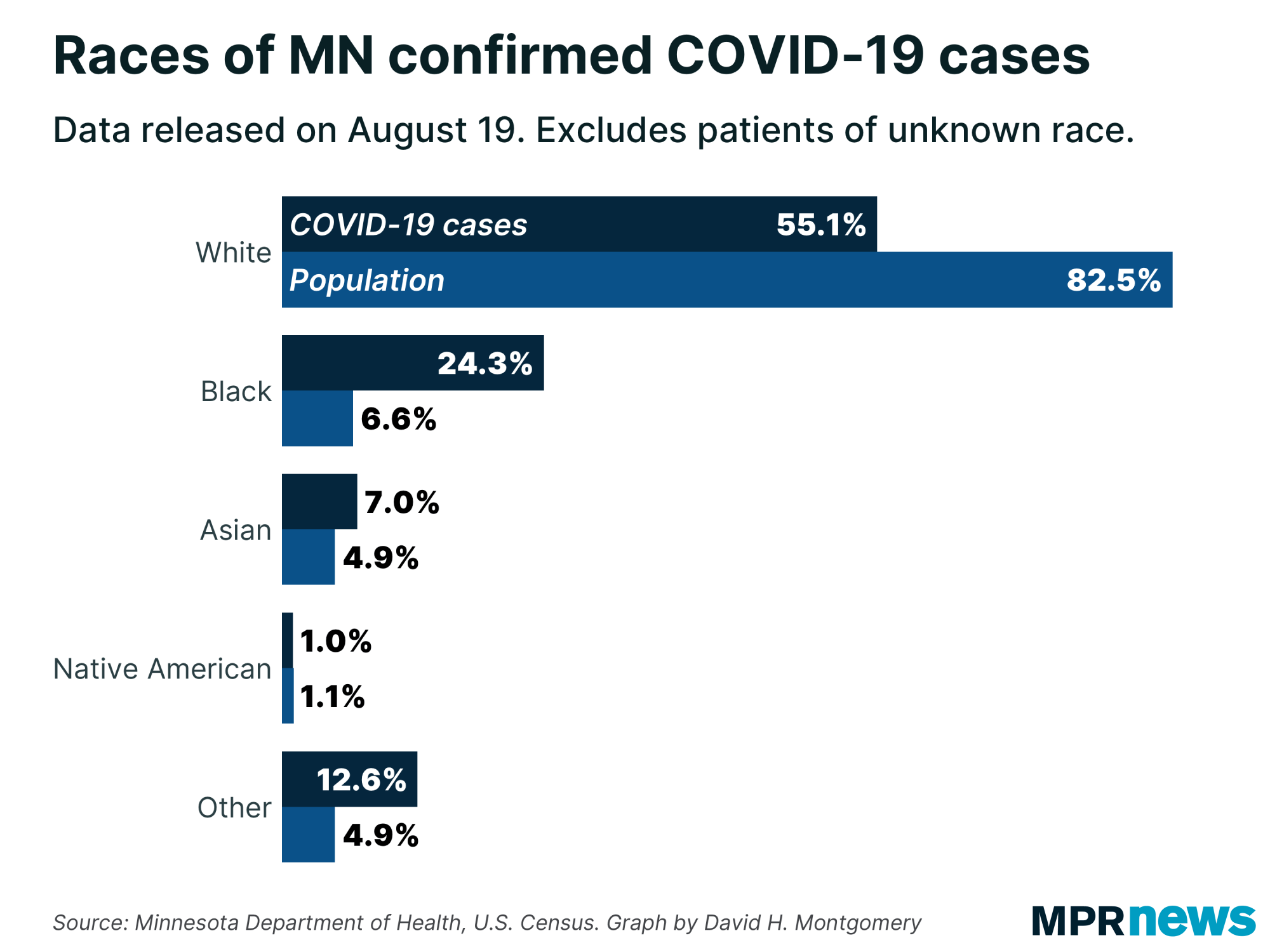
Public health officials expect people of color in the state to be hit harder by the novel coronavirus than white Minnesotans because many of the preexisting health conditions that can make the virus more deadly — asthma, high blood pressure, cardiovascular disease — are more prevalent among certain racial and ethnic groups.
“The important thing that we like to make clear is that it’s not because of a biological difference between races,” said Andrea Westby, a family medicine physician at North Memorial Health Hospital. “It actually has more to do with historic oppression.”
Racial bias and opportunity barriers can affect a person’s health in many ways. African Americans are more likely to be uninsured and working low-paying jobs. And poverty can make it difficult to socially isolate to avoid contracting the virus, particularly for people who live in dense housing or rely on public transportation. Some low-wage workers with the highest exposure risks are personal care attendants and home health aides, said Westby.
“Most of the people who are doing that work — women and women of color, in particular — we’re going to see more exposures,” said Westby. “Because that type of work can’t be done from home.”
It is especially difficult to shelter in place or practice self isolation, when a person has nowhere to live.
According to a 2018 survey conducted by Wilder Research, African Americans and Native Americans are overrepresented in the ranks of the homeless. The survey also found that most homeless adults have chronic illnesses.
“We have essentially decades of data that tell us homelessness is worse for your health than a majority of our usual chronic conditions combined,” said Dr. Danielle Robertshaw, who has worked with homeless populations for 20 years.
State and county emergency orders have made homeless people more reliant on shelters since many public buildings homeless people relied on for bathrooms or recreation are now closed, said Robertshaw, who practices at Hennepin Healthcare.
Hennepin County has acquired isolation hotel rooms to help homeless people housed in shelters.
Robertshaw said there are two different groups staying in the rooms.
One group contains people who are not symptomatic, but are vulnerable given their age and health status.
The other group is made up of people who have tested positive for COVID-19 or are symptomatic and need to be isolated during testing.
Robertshaw said initially she worried that the county would run out of these rooms because it often took five to seven days to get test results. Now results come back in less than a day.
“Certainly if we have a negative test and we can help someone discharge safely from the hotel and not be at risk of spreading to the community, that’s a lot faster turnaround,” she said.
Ramsey County also reopened a vacant building with 140 beds for homeless people who need to be isolated in order to avoid contracting or spreading the virus.
It’s not clear what impact these mitigation efforts have had because it’s still early in the pandemic.
Fewer than 1 percent of infections have come from people living in homeless shelters, according to Minnesota Department of Health data. But the population is small. Wilder Research said more than 50,000 people experience homelessness in 2018 — a total far lower than 1 percent of Minnesota’s total population.
COVID-19 will have lasting impacts on all of society, but especially in communities that weren’t whole before the pandemic hit, said Rachel Hardeman, an assistant professor at the University of Minnesota’s School of Public Health. Her research focuses on reproductive health and how long-term exposure to racism wears on black women and contributes to higher rates of death for them and their newborns.
Hardeman worries the pandemic is just one more stressor that will amplify and prolong the inequality which has disproportionately sickened African Americans.
“We are going to see some of the implications for decades to come,” said Hardeman. “Both, I think, as a society and our communities, but also physiologically in respect to health and well-being.”


